Next-generation endovascular coils and adjunctive coiling techniques
Once a brain aneurysm ruptures, prognosis is dour, meaning prevention is key. Thrombolic Stroke
Historically, brain aneurysms have been treated with surgery, but endovascular approaches are more widely used today.
Coiling, stenting, and PED placement are all effective and minimally invasive ways to prevent brain-aneurysm rupture.
In March 2023, the actor Tom Sizemore, known for his intense performances in films like Natural Born Killers and Saving Private Ryan, died after being taken off life support. On February 18, 2023, he collapsed in his home due to a stroke and was later diagnosed with a brain aneurysm. He remained in a coma in the ICU until his death. He was 61 years old.
Sizemore’s outsized life was plagued with legal troubles and drug abuse. From media accounts, it’s unclear what role his previous medical history played in his stroke and aneurysm. His death, however, shone a light on brain aneurysm and what preventions are available for this deadly condition.
Brain aneurysms are a potentially life-threatening medical condition caused by the weakening of the walls of blood vessels in the brain. They are relatively common, with an estimated 2% to 5% of the population affected.[] Traditionally, open surgery was the only option for treating brain aneurysms. However, in recent years, major advances have been made in endovascular treatments for brain aneurysms.
The rupture of a cerebral aneurysm can lead to considerable morbidity and mortality, making early detection and treatment essential.
According to a study by Etminan and colleagues, the overall mortality rate after an aneurysmal subarachnoid hemorrhage (aSAH) is approximately 30%,[] with a high rate of disability in survivors. The study found that factors associated with a higher risk of mortality after aSAH include older age, male gender, poor neurological grade at presentation, and the presence of intraventricular hemorrhage.
Another study by Nieuwkamp and colleagues found that patients who survived aSAH had a high risk of long-term disability, with nearly 19% of all survivors experiencing significant impairments in physical, cognitive, or emotional functioning.[]
Brain aneurysms cause serious complications when they hemorrhage and thus damage the brain. Only 25% of patients with a ruptured brain aneurysm recover well. Consequently, the key is to catch brain aneurysms before they rupture.
From a historical perspective, surgery was used to correct these aneurysms before they rupture. Surgery, however, is burdensome, according to neurosurgeon Mark Bain, MD, remarking in a Cleveland Clinic podcast.
From a surgical perspective, the patient would require a large incision, a “bad-looking haircut,” substantial bone shaving, microscopic visualization, and the placement of a small aneurysm clip, which pinches off circulation to prevent interface with blood and aneurysm rupture.[]
“It was a very, very effective treatment,” he said.
“We could pretty much treat all aneurysms in the brain with this treatment, but it carried with it a lot of recovery time, a fair amount of morbidity, so a lot of patients that we did this operation to simply didn't get back to their normal lifestyles afterwards.”
— Mark Bain, MD, Cleveland Clinic
“So obviously,” Dr. Bain added, “there was a need to improve on these technologies. People just didn't want to have these treatments, these open surgical procedures done. As most fields of medicine have done, things have gone more in a minimally invasive fashion, and I think neurosurgeons, neurologists, in fact, really a lot of neurointerventional radiologists sort of picked up from the cardiologists and how they're placing stents in the heart through endovascular inside the blood vessel techniques. We saw these approaches and said, ‘Hey, listen, can we do this?’”
In the 1990s, the Guglielmi detachable coil system emerged, which introduced a modern era of neurointervention and endovascular neurosurgery, as noted in a review in Stroke & Vascular Technology.
Although the outcomes of early coil intervention left much to be desired, with high occlusion rates, advancements in coil properties improved outcomes to where coils outperformed clipping in terms of morbidity and mortality.[]
Advances in coil technology included the adoption of different lengths, pliability, shapes, coating, detachment zones, and devices that augmented their use.
From a mechanistic perspective, the aneurysm is filled with a small platinum coil or coils, which causes the blood to clot, consequently destroying the aneurysm, according to the Brain Aneurysm Foundation.[] Patients would be discharged from the hospital after a day with a bandage on their groin or wrist. They could return to work in 2 days, which is a far cry from open surgical intervention. Dr. Bain estimates that about 90% of aneurysms are treated in minimally invasive fashion—from inside the blood vessel.
Next-generation endovascular coils and adjunctive coiling techniques
A full review of all the endovascular advances centered on coiling is outside the scope of this article. Instead, here are some notable advances.
This intervention involves the temporary inflation of a balloon catheter across the aneurysm neck during coil placement. The balloon increases coil packing density and is recovered at the end of the procedure. During the procedure, the balloon catheter temporarily occludes the parent artery in case the aneurysm ruptures. The goal of balloon remodeling is to provide a more stable and uniform surface for the placement of the coil or coils, reducing the risk of coil protrusion or displacement, which can lead to rupture or recurrence of the aneurysm. Balloon remodeling can also help to reduce the amount of contrast agent required for imaging during the procedure and reduce the risk of coil prolapse, thromboembolic events, and vessel rupture.
However, the technique does carry some risks, including vessel dissection or rupture, thromboembolic events, and perforation of the aneurysm. Repeated inflation and deflation of the balloon can also result in intimal injury. Nevertheless, research has demonstrated that the safety of balloon remodeling is akin to conventional coiling.[]
“It is thought that balloon remodeling may simplify the process of endovascular coiling and reduce the risk of complication by reducing total procedure time. ”
— according to the authors of the Stroke & Vascular Technology review.
Authors of a review article in the British Journal of Radiology offer further perspective.
“Since coiling’s introduction, recanalization and retreatment have been a concern. Key factors include aneurysm location, diameter and neck size. Balloon-assisted coiling (BAC) was one of the first major developments in technique that remains popular and prospective, multicentre evidence, for example, Analysis of Recanalization after Endovascular Treatment of Intracranial Aneurysm (ARETA) support the popularity, safety and feasibility of coiling. BAC offers higher packing density and control of proximal vessel flow,” they wrote.[]
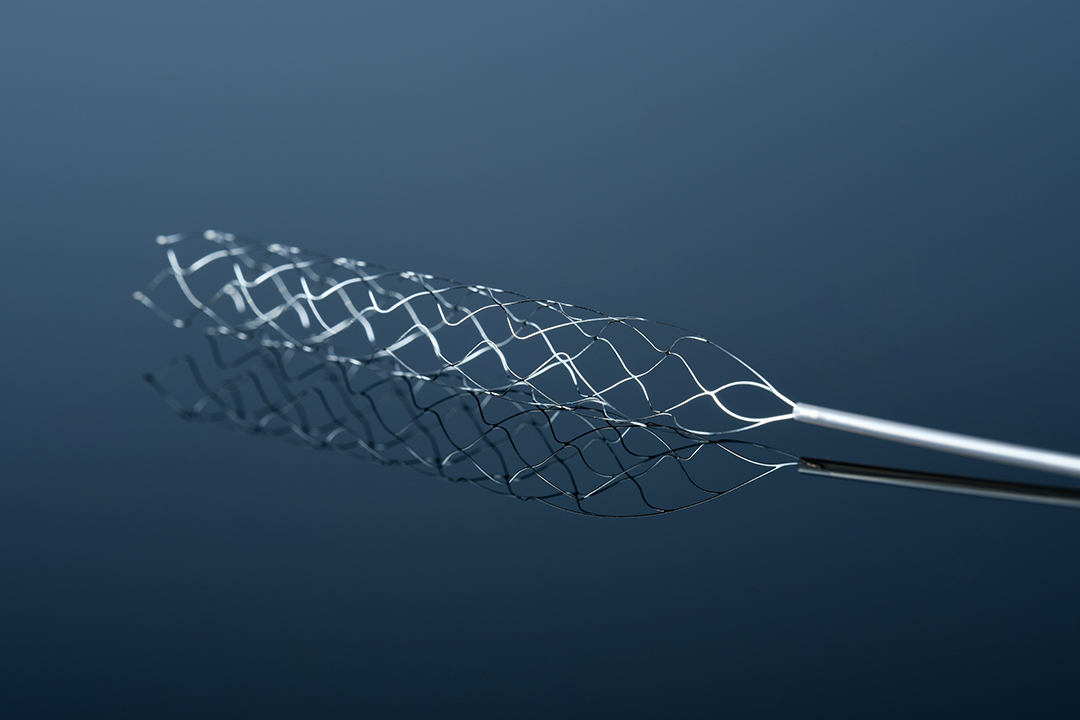
A stent is a small, mesh-like metal tube made of metal alloys such as nitinol, stainless steel, or cobalt-chromium. Stents are used in the endovascular treatment of cerebral aneurysms. These materials are chosen for their strength, flexibility, and biocompatibility. Nitinol is a particularly popular choice for stents due to its shape memory and superelasticity properties. These properties allow for the stent to be compressed for delivery through the catheter and then expanded to its original shape once deployed within the blood vessel.
When used in conjunction with coiling, stents can help to provide additional support and stability to coils, reducing the risk of complications and improving the overall success of the treatment.
Stent-assisted coiling involves the insertion of a stent into the parent artery—across the neck of the aneurysm—prior to coil placement. The stent is then deployed, providing a scaffold for the coils to adhere to, and helping to prevent coil migration or prolapse into the parent artery. Coils are particularly helpful with large aneurysms, which were once very challenging to treat endovascularly. Like coils, stents are placed via catheter in an artery at the level of the groin and can be placed at the same time as a coil. Patients require anti-aggregate treatment.
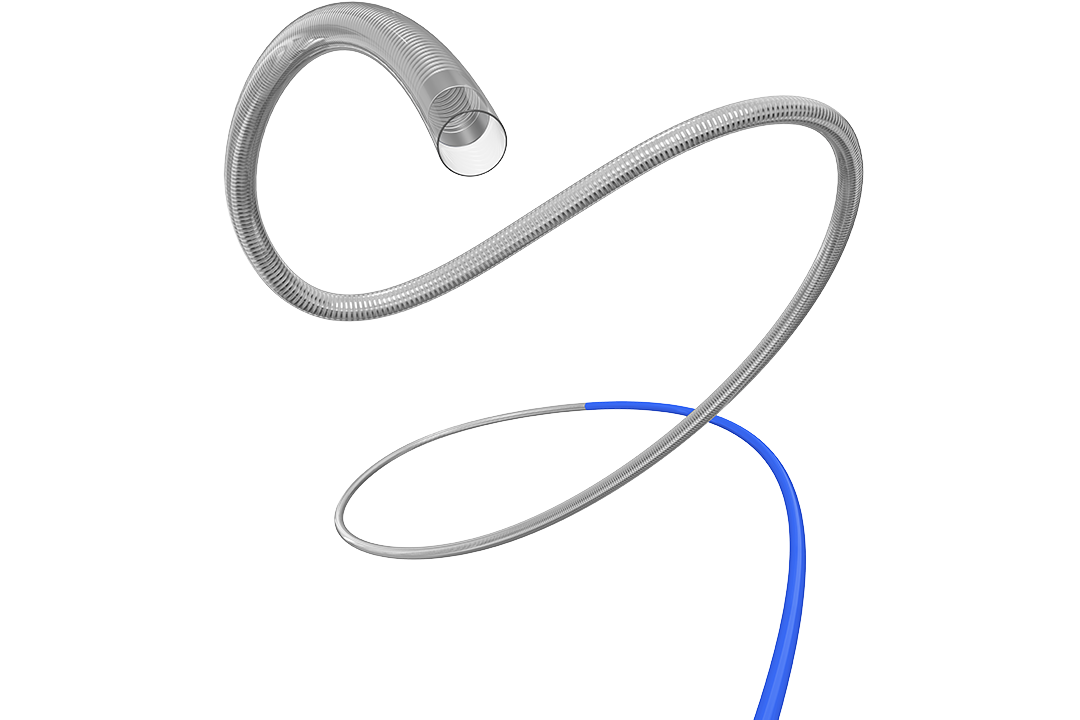
The Pipeline Embolization Device (PED) is a self-expanding cylindrical stent made of platinum, tungsten, and cobalt-chromium-nickel-molybdenum alloy, which was granted approval by the FDA in 2011 for the treatment of large and complex cerebral aneurysms.
The device consists of 48 individual strands densely braided into a wire mesh tube, which is delivered to the aneurysm through a microcatheter and is positioned across the neck of the aneurysm. It is then expanded, diverting blood flow away from the aneurysm and promoting organization of the thrombus within the aneurysm lumen. Complications include device migration, postoperative SAH, intraparenchymal hemorrhage, and small perforator infarctions.
What this means for you
The advancements in the endovascular treatment of cerebral aneurysms offer exciting new options for managing this potentially life-threatening condition with minimally invasive techniques that have excellent outcomes and reduced risk of complications compared with open surgery. However, it is important for physicians to remain vigilant in prevention efforts by addressing modifiable risk factors, promoting early detection and management of aneurysms, and raising awareness of the signs and symptoms of aneurysms.
© 2023 M3 USA Corporation. All Rights Reserved.
Nerve Claudication © 2023 M3 USA Corporation. All Rights Reserved.